Má ég gera ţetta svona til kynningar á nýrri tćkni? Ţetta er einnig auglýsing fyrir greinina.
How artificial intelligence helps get new treatments to patients.
https://www.reuters.com/brandfeatures/intelligent-regeneration-in-japan
Regenerative medicine is a promising field, with the potential to revolutionize medical treatments by restoring damaged tissues and organs.
1
klikka mynd stćrri
2
In Japan, experts are focusing on the development of induced pluripotent stem cells (iPSCs), which are a novel means to treat a range of degenerative conditions, including those leading to vision loss.
This ground-breaking work is only possible thanks to the support of the country’s government and a series of recent reforms. Professor NISHIDA Kohji, research lead at the Ophthalmology Laboratory at Osaka University, explains:
“In Japan, there are many talented stem cell researchers. Funding from the government helps them to train, conduct further research and, hence, continue to innovate in this field.”
As a result, a number of significant breakthroughs have recently been realized as Japan’s researchers endeavor to produce iPSCs on a scale where every patient has access to regenerative treatments.
Breakthrough #1:
Reconstructing the cornea
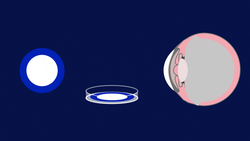
The loss of corneal epithelial stem cells leads to sight loss as the cornea, which sits at the front of the eye, becomes covered by a membrane called the conjunctiva. A corneal transplant is a standard treatment, but a lack of donors and rejection of the transplanted tissue limit the number of patients who benefit.
Osaka University recently conducted the world’s first iPSC transplant, using artificially derived stem cells, on a patient with corneal disease. This treatment succeeds where others have failed because it replicates whole-eye development thanks to the use of artificial intelligence (AI) techniques.
3
Clinical trials have started to standardize this treatment and there is a clear roadmap in place, as Professor Nishida explains:
“We want to move this treatment from research into medicine using a multi-center clinical study. We predict this will take four or five years to complete.”
Breakthrough #2:
Robotic labs
To give every patient access to regenerative treatments, researchers need to be able to grow iPSCs on a large scale, as well as derive diverse cell types from iPSCs. But these cells are very delicate and fragile, and the researchers who cultivate them by hand need to be as skilled as any craftsperson. Only a handful of highly experienced researchers possess the necessary skills to conduct this is specialized and complex procedure.
4
Two teams are developing AI-enhanced robotics to address this challenge. These machines are trained to replicate the skills of these experienced researchers.
5
6
At the RIKEN Institute, researchers have replicated the procedures to generate retinal cells. These machine-cultured cells display the same quality as manually cultured cells, showing that iPSC-derived cells can be successfully grown by an automated process.
7
All the team staff are looking into the future with due awareness
of the importance of living in harmony with robots and AI,” Ins
according to Dr. KANDA Genki, a research scientist at RIKEN.
The technique could also easily be extended to all lab-grown cells as the lessons learned by one robot can be copied to other robots. As a result, this AI-enabled robotics technique could enable the widespread cultivation of iPSC-based regenerative treatments for a range of disorders.
8
9
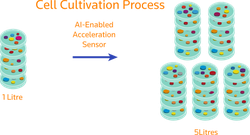
The lab has seen many successes. For example, an AI-enabled acceleration sensor was recently developed to improve the stability of the delicate cell cultivation process. Usually, cells are cultured in one litre or less but, by mixing gently thanks to the feedback from the sensor, billions of iPSCs can now be cultured on a five-litre scale.
10
Breakthrough #3:
Consistent, quality cells
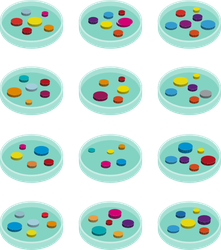
Researchers from Nagoya University have worked in collaboration with Nikon to design an image analysis system to evaluate the quality of iPSCs for their further use both in drug and treatment applications.
11
The AI-based cell quality prediction system is non-invasive and, effectively, learns as a human does, continually optimizing its analysis techniques as it conducts more cell evaluations. What’s more, and unlike manual evaluations, the system can also quantify the quality of the iPSCs.
This ability to measure cell quality is an important but often overlooked step during the development of regenerative treatments, as Professor KATO Ryuji, associate professor at Nagoya University, explains: “Thinking of quality in regenerative medicine products, we tend to focus on its effectiveness and safety. But we sometimes forget another quality that is required for regenerative medicine products. That is consistency.”
12
Such consistency is difficult to achieve using manual techniques at the commercial scale because the production of live cell cultures is still technologically difficult. “So, to effectively control the process in manufacturing to achieve consistency, AI technology is both important and powerful to assist the automation of cell cultures,” Kato explains.
The consistent quality of manufactured iPSCs is not only a vital factor to cultivate these cells in a safe and effective manner, it is also one of Japan’s major research strengths.
Looking Ahead
The field of regenerative medicine is going from success to success in Japan. Thanks to the country’s existing engineering prowess, a range of AI-enabled techniques are now under development to democratize these cutting-edge regenerative treatments.
“In stem cell science, our country is certainly leading both the scientific findings and the clinical applications of iPS cells. The Japanese technologies from the robotics and automation industries are now rapidly integrating in this field… such engineering technologies from Japan would change the worlds’ cell culture for regenerative medicine,”
Professor Kato explains
Unlike their manual counterparts, machine-aided techniques are fiscally feasible at a commercial scale and provide increased productivity.
“If we want to lower the cost of regenerative treatments, we need to enable large scale production using artificial intelligence techniques,”
Professor Kino-oka explains.
Thanks to artificial intelligence, researchers can now develop new regenerative medicines, start to consistently, cost-effectively and safely cultivate these transplantable cells at scale to reach human patients in need.
display the same quality as manually cultured cells, showing that iPSC-derived cell
13
Bloggar | Slóđ | Facebook | Athugasemdir (0)







 agny
agny